Fortunately, there are companies that will give someone a guaranteed issue whole policy. There NO health questions asked. How much does it cost? Typically a person will pay roughly 30% more for this type of policy. The main point is that you CAN get life insurance. It is still affordable. Whole life is often referred to as permanent insurance. It does build cash value in 18-24 months. You can even use the cash value to pay some of the premiums if you get in a jam financially. Here is how a guaranteed whole life insurance policy works: These policies are “graded”. For example, if you purchased $10,000 for a face amount and you passed away during the first 2-3 years of owning the policy, your beneficiary would get 100-110% of the premiums you have paid in. After the 2-3 “graded” period if you pass away they would receive the whole $10,000.
Fortunately, there are companies that will give someone a guaranteed issue whole policy. There NO health questions asked. How much does it cost? Typically a person will pay roughly 30% more for this type of policy. The main point is that you CAN get life insurance. It is still affordable. Whole life is often referred to as permanent insurance. It does build cash value in 18-24 months. You can even use the cash value to pay some of the premiums if you get in a jam financially. Here is how a guaranteed whole life insurance policy works: These policies are “graded”. For example, if you purchased $10,000 for a face amount and you passed away during the first 2-3 years of owning the policy, your beneficiary would get 100-110% of the premiums you have paid in. After the 2-3 “graded” period if you pass away they would receive the whole $10,000.Congestive heart failure (CHF) undermines the heart’s job of pumping blood around the body. Over time, this failing causes the organs to receive less blood.
In this article, we look at how CHF progresses over time and what the outlook is for people with this condition. We also examine the causes, symptoms, and treatment options.
Stages
There are four different stages of heart failure: A, B, C, and D.
Progression to the next stage is linked with a reduction in 5-year survival rates.
Stage A
High risk of developing HF due to having other conditions strongly associated with HF developing.
Examples of these conditions include chronic high blood pressure, diabetes, and coronary artery disease.
People at this stage have no problems with the structure of the heart or how their heart works. They will have also never shown any signs or symptoms of HF.
Stage B
People at this stage will have developed structural heart disease that is strongly linked to the development of HF. This includes having an enlarged left ventricle or having had a heart attack.
However, people at this stage will still have never shown any signs or symptoms of HF.
Stage C
People at this stage will be showing or will have shown symptoms of HF linked to underlying structural heart disease.
This category includes those who are experiencing fatigue or difficulty breathing due to a problem with the left ventricle contracts. It all also include people who no longer show symptoms but are currently undergoing treatment for previous symptoms of HF.
People at this stage will have advanced structural heart disease and will display significant symptoms of HF even when at rest.
This stage is very serious and requires special treatments, such as mechanical circulatory support, continuous inotropic infusion, cardiac transplant, or hospice care.
Types
The most common type of CHF is left-sided CHF, which occurs when the left ventricle of the heart cannot pump blood effectively to the rest of the body. This can cause fluid to build up in the lungs and make breathing difficult as it progresses.
There are two kinds of left-sided heart failure:
- Systolic heart failure, when the left ventricle cannot contract normally, limiting the heart’s ability to pump blood to the rest of the body.
- Diastolic failure, when the muscle in the left ventricle stiffens. If the muscle cannot relax, the heart ventricle will not be able to fully fill with blood between heartbeats.
Right-sided CHF is less common. It happens when the right ventricle has cannot pump blood to the lungs as effectively. This can lead to the blood backing up in the blood vessels, which may cause fluid retention in the lower legs and arms, abdomen, and other organs.
A person can have left-sided and right-sided CHF at the same time. However, CHF usually begins on the left side and spreads to the right side if left untreated.
Outlook
Symptoms of CHF vary in severity but tend to get worse over time.
Lifestyle strategies can reduce the risk of CHF and can also slow its progress. In fact, many people with mild or moderate CHF find that lifestyle remedies are enough to control their symptoms.
Lifestyle strategies, such as exercising and maintaining a healthy weight, are sometimes enough to prevent or slow the progression of mild CHF.
To prevent or slow the progression of CHF:
- maintain a healthy weight
- get enough exercise – some people may need to follow a modified exercise regime in consultation with a doctor
- manage stress through meditation, therapy, and other healthy methods
- eat a heart-healthy diet low in trans fats, rich in whole grains, and low in sodium and cholesterol.
- monitor blood pressure regularly
- get vaccinated for the flu and pneumococcal pneumonia
Additionally, people who already have CHF should avoid caffeine, get adequate rest, track changes in their symptoms, avoid very cold or hot temperatures, and wear loose-fitting clothing.
Left untreated, CHF can be fatal. Even with adequate treatment, CHF may get worse over time, triggering problems throughout the body.
Causes
CHF is more likely to occur in people who have other conditions that weaken the heart. The risk is also increased by several lifestyle factors that are bad for the heart.
Risk factors for CHF include:
- congenital, appearing early in children and infants
- high blood pressure or cholesterol
- obesity
- asthma
- chronic obstructive pulmonary disease and coronary heart disease
- other cardiovascular conditions
- heart infection
- reduced kidney function
- a history of heart attacks
- irregular heart rhythms
- abuse of alcohol or drugs
- smoking
- older age
Definition
CHF describes a cluster of symptoms, not a single disease.
The American College of Cardiology and the American Heart Association define heart failure according to how it has progressed. This classification is not meant to replace the New York Heart Association functional classification system but rather complement it.
When the kidneys are deprived of good blood supply, they struggle to filter fluids to make urine. This causes fluid to build up in parts of the body, particularly in the liver, eyes, lungs, and legs. Congestive heart failure gets its name from the “congestion” of this excess fluid.
Symptoms
People with a history of cardiovascular health issues or several risk factors for CHF should seek immediate care if they experience symptoms of CHF. Similarly, if symptoms do not improve after a few days, a person should see a doctor.
The most common symptoms of CHF are:
- Shortness of breath or difficulty breathing: People with CHF may also struggle to breathe when lying down due to fluid accumulation in the lungs.
- A persistent, unexplained cough: Some people experience wheezing and pink or blood-stained mucus.
- Swelling in the legs, ankles, abdomen, or hands: The swelling may get worse as the day goes on or after exercise.
- Feeling tired: This can happen even when someone is well-rested.
- Changes in thinking and memory: Electrolyte imbalances due to CHF can impair the ability to think clearly.
- Nausea: This can be accompanied by a drop in appetite.
- A rapid heart rate: This occurs because the heart is unable to pump blood with a regular rhythm.
- Feeling light-headed or dizzy: This might also include tingling or numbness in the extremities due to an inadequate blood supply.
As the fluid builds up, people with CHF may develop painful swelling. This is called edema and was once referred to as dropsy.
Swelling caused by CHF can undermine the movement, and may even cause dangerous blood clots in the legs. Also, organs affected by fluid retention may not work properly, making it harder to breathe or exercise.
Children with CHF may experience delays in physical development, while babies with the condition may struggle to gain weight.
Diagnosis
A doctor or cardiologist will perform a physical exam. This may involve listening to the heart for abnormal heart rhythms. They may also order other diagnostic tests, including:
- Electrocardiogram (EKG or ECG), which records the heart’s rhythm.
- Echocardiogram, which can determine if a person has poor blood flow a heart muscle that is not functioning properly.
- Stress tests, which show how the heart performs under different levels of cardiac stress, such as running on a treadmill.
- Blood tests, to look for infections and a person’s BNP level. BNP is a hormone that increases with heart failure.
- MRI, which can be used to take pictures of the heart.
- Cardiac catheterization, which can show blockages in the arteries. This may be done at the same time as checking blood flow and pressure in the ventricles.
Treatment
Different medications can help the symptoms of CHF. These include:
- Blood thinners to reduce the risk of blood clots, which might break loose and travel to the heart, lungs, or brain. Blood thinners can also increase bleeding.
- Angiotensin-Converting Enzyme (ACE) inhibitors to widen blood vessels, making it easier for the heart to pump blood around the body. ACE inhibitors can also lower blood pressure.
- Anti-platelet drugs used to stop blood clots by preventing platelets in the blood from sticking together.
- Beta-blockers, which lower the heart rate and reduce the force with which the heart must pump. They can also lower blood pressure.
- Statins, which are used to lower “bad” LDL cholesterol, and may raise “good” HDL cholesterol.
- Calcium channel blockers, prescribed to help the heart pump less forcefully. They can also control irregular heart rhythms.
- Diuretics to help the body excrete more fluid in the urine and prevent it from overwhelming the heart and lungs. They also reduce swelling and prevent shortness of breath.
- Vasodilators reduce the amount of oxygen the heart needs to dilate. Vasodilators can also ease chest pain.
In people with advanced CHF, medication and lifestyle changes alone may not be enough. Medical procedures that can help include the following:
The placement of implantable devices
- An implantable defibrillator can prevent heart arrhythmias.
- A pacemaker can address electrical problems in the heart to help the ventricles contract more regularly.
- A left ventricular assist device (LVAD) can support the pumping ability of a heart when it cannot do this efficiently on its own. LVADs were once used on a short-term basis, but can now be a part of long-term treatment.
Other procedures
There are a number of other procedures a doctor may recommend to treat CHF:
- Angioplasty to open a blocked artery: Sometimes the doctor will place a stent to help the vessel remain open.
- Coronary artery bypass surgery: This reroutes some of the blood vessels so the blood can travel around the body, avoiding diseased or blocked blood vessels.
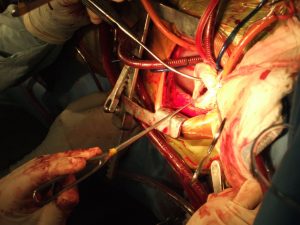
- Valve replacement surgery: A doctor will replace an inefficient or diseased valve with a mechanical valve or one grown from living tissue.
- Heart transplant: This may be the only option in people with severe CHF that is not well managed with other therapies.
Not everyone with CHF is a candidate for a transplant, and the wait for one can be long.
A recipient must be healthy enough for the surgery. Surgery on the heart can be extremely dangerous, so doctors typically urge people to attempt lifestyle remedies and take medication before trying heart surgery or implantable devices.
A lot of people are diagnosed each year with this condition. There are treatments available but no cure. This condition can be better managed with lifestyle changes. One of the things we worked on during a physical therapy treatment was increasing endurance and strength. Also teaching on proper elevation for the lower extremities. Most patients I had did well with their physical therapy treatments. This has been an overview of congestive heart failure and life insurance with heart failure. Is there life insurance for someone with heart disease?

References
https://medlineplus.gov › Health Topics